Abstract

Ectopic expression of transcription factor HoxB8 in murine bone marrow stem cells programs cells to stably expand exponentially in culture. When HoxB8 expression is regulated through a conditional promoter, cells are capable of expansion through HoxB8 induction or differentiation into neutrophil-like cells through HoxB8 withdrawal. We have previously demonstrated that some derivations of HoxB8 progenitor cells are capable of engraftment in an unconditioned murine host leading to rapid formation of a transient population of donor neutrophils in the periphery. Donor derived neutrophils (ddN) function comparably to host wild-type (WT) neutrophils ex vivo. Based on these findings, we hypothesize that conditionally immortalized HoxB8 progenitor cells have the potential to serve as a novel neutrophil driven cellular therapy.
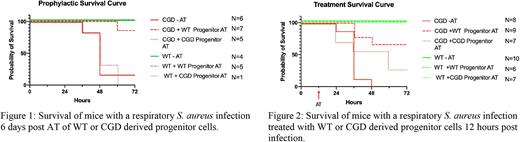
To investigate the use of HoxB8 progenitor cells as a cellular therapy for disease, we utilized a well characterized murine model of the congenital disorder CGD. Individuals with CGD are particularly susceptible to infections with Staphylococcus aureus due to loss of reactive oxygen species (ROS) production via the NADPH oxidase. Impaired neutrophil function leads to increased inflammation and decreased microbial killing. We found that prophylactic treatment of CGD mice with an adoptive transfer (AT) of WT HoxB8 progenitor cells protected them from an otherwise lethal pulmonary infection (Figure 1). Mice which received an AT of progenitor cells derived from a CGD animal did not have improved outcomes. This suggests the effector functions of the WT ddN were responsible for the change in survival. To better understand the mechanism of protection derived from the AT, we developed a novel fluorescent killing assay. This assay demonstrated the positive influence of the WT ddN on the host CGD neutrophils intracellular killing capacity in vivo.
In addition to prophylactic treatment, post infectious treatment with the progenitor cells improved survival to >50% (Figure 2). Interestingly, twelve hours post adoptive transfer, donor derived cells represent a small population of the BAL cellular environment (<1%). Evaluation of the BAL and serum cytokine environment at this time-point provide insight to the immuno-modulatory role of the donor derived cells.
Results from this study demonstrate the promise of a neutrophil progenitor based cellular therapy. This approach is unique from those currently employed as progenitor cells engraft without conditioning, expand and differentiate in vivo unlike granulocyte transfusions, and may be genetically modified in culture to potentially address the challenges of microbial resistance genes.
Disclosures
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal